Impulsa la Salud Digital con Asociaciones Público-Privadas (McKinsey)
Impulsa la Salud Digital con Asociaciones Público-Privadas (McKinsey)
17 dic 2025

¿No sabes por dónde empezar con la IA?
Evalúa preparación, riesgos y prioridades en menos de una hora.
¿No sabes por dónde empezar con la IA?
Evalúa preparación, riesgos y prioridades en menos de una hora.
➔ Descarga nuestro paquete gratuito de preparación para IA
La nueva investigación de McKinsey describe cómo las asociaciones público-privadas (APP) realmente escalon digitalmente la salud: comienza con una justificación clara (capacidad, escala o financiamiento), elige el actor privado adecuado, y diseña de antemano la propiedad, adquisición, privacidad de datos y sostenibilidad. Las lecciones de Canadá, Estonia, México, Tanzania y Togo muestran qué funciona—y por qué.
Puntos clave
Capacidad, escala, financiamiento: Los gobiernos suelen involucrar socios privados por sus capacidades técnicas únicas (100% de los casos), escala (83% en ecosistemas maduros) o financiamiento (48% en contextos limitados).
Upside económico comprobado: Las herramientas digitales pueden desbloquear hasta un 15% de eficiencia en los sistemas de salud de países de ingresos bajos y medios para 2030 al desplegarlas a gran escala.
Mecanismos reales, no eslóganes: La adquisición directa, centros de innovación, participaciones accionarias y la propiedad por fases ayudan a alinear incentivos y sostener soluciones.
Cinco lecciones que se repiten una y otra vez
Guía sobre dónde invertir. Usa un mapa de ruta nacional de salud digital y clarifica la propiedad para reducir la fragmentación (por ejemplo, Connect Care de Alberta con Epic).
Involucra al actor adecuado. Afya-tek de Tanzania mezcló herramientas para CHW y flujos de trabajo farmacéuticos al asociarse con D-tree/AHAI para obtener experiencia y financiamiento.
Crea incentivos. Reducciones fiscales, subvenciones y centros de innovación (por ejemplo, la comunidad HealthTech de Estonia; CAN Health en Canadá) aceleran la calidad y adquisición.
Construye confianza con salvaguardas. Aplica normas alineadas con el GDPR (Estonia PDPA) y requiere supervisión para acceder a conjuntos de datos sensibles (por ejemplo, biobanco FINBB).
Planea la sostenibilidad. Utiliza financiamiento no público donde sea necesario, participaciones accionarias para alinear incentivos (Unity Health Toronto × Signal 1), y transiciones de propiedad por fases (por ejemplo, m-mama, CHIS de Togo).
McKinsey también señala: el gasto del sector privado representa 40–60% del gasto en salud en muchos países de ingresos bajos y medianos, y la inversión privada en salud digital alcanzó los $25.1 mil millones en 2024—resaltando por qué las APP son importantes. McKinsey & Company
Pasos prácticos o ejemplos (un manual que puedes usar)
Comienza con el “por qué”. ¿Estás comprando capacidad (triaje de IA, implementación de EHR), escala (despliegue nacional) o financiamiento (capital combinado/donante)? Escribelo; esto guía la selección del modelo.
Elige el modelo.
Adquisición directa para sistemas críticos y estandarizados.
Centros de innovación y entornos de prueba para pruebas rápidas.
Modelos de acciones/cuotas para alinear incentivos para la IA co-desarrollada o análisis.
Decide propiedad y supervisión temprano. Separa la propiedad de la solución del IP, define la supervisión conjunta o única, y establece un camino de transición (privado→conjunto→público) para construir capacidad pública.
Desmitifica los datos desde el primer día. Codifica la privacidad, el acceso y la auditoría; enlaza la elegibilidad de adquisición con el cumplimiento de leyes/estándares nacionales.
Financiación para la durabilidad. Combina líneas presupuestarias con capital privado/donante; usa pagos diferidos o tarifas basadas en volumen para suavizar el flujo de efectivo.
Mide lo que importa. Rastrea la adopción (pacientes/profesionales de la salud), costos para servir, reducciones de tiempo de espera e impactos en la equidad; el manual de adopciones de McKinsey muestra las fases de configuración → escalamiento → mejora de beneficios que mejoran la adhesión.
Ejemplos vivos para hacerlo tangible
Receta electrónica de Estonia: nacional, integrada con EHR y sistemas nacionales—recetas digitales casi universales.
Unity Health Toronto × Signal 1 (Canadá): el hospital toma una participación minoritaria; actúa como un “laboratorio viviente” para monitoreo de IA (CHARTWatch).
COVID360 de Ciudad de México: asociación público-fundación para establecer rápidamente una plataforma de tratamiento durante COVID-19.
Tanzania Afya-tek: conecta a trabajadores de salud comunitarios, instalaciones y dispensarios—adquirido a través de un mapa de ruta; construido para interoperabilidad.
La última guía de McKinsey muestra que las asociaciones público-privadas escalan la salud digital cuando los gobiernos definen el “por qué”, eligen el actor privado adecuado, aseguran el financiamiento/propiedad, aplican salvaguardas de datos y planean para la sostenibilidad—utilizando mapas de ruta, incentivos y propiedad por fases para alcanzar la escala nacional. McKinsey & Company
Preguntas frecuentes
¿Qué son las asociaciones público-privadas en salud digital?
Colaboraciones estructuradas donde gobierno y actores privados (con y sin fines de lucro) co-diseñan, construyen u operan soluciones de salud digital—a menudo con financiamiento mixto y supervisión compartida. McKinsey & Company
¿Por qué estas asociaciones son importantes ahora?
Porque las brechas de capacidad, escala y financiamiento persisten—especialmente en países de ingresos bajos y medios donde el gasto privado es el 40–60% del gasto en salud y la inversión digital está en aumento. McKinsey & Company
¿Cómo funcionan las asociaciones en la práctica?
Los modelos comunes incluyen adquisición directa, centros de innovación, estructuras de acciones o tarifas y propiedad por fases; el éxito depende de la privacidad de datos, adquisición transparente y mapas de ruta claros. McKinsey & Company
¿Cuál es el valor potencial?
En países de ingresos bajos y medios, las herramientas digitales escaladas podrían desbloquear hasta 15% de ganancias de eficiencia del sistema; la OMS estima que incluso la inversión digital modesta por paciente puede salvar más de 2 millones de vidas por enfermedades no transmisibles con el tiempo. McKinsey & Company
Resumen
El mensaje de McKinsey es pragmático: trata las APP como problemas de diseño. Elige el modelo que coincida con tu “por qué”, incorpora gobernanza y privacidad, financia para el largo plazo y establece un mapa de ruta de adopción (configuración → escalamiento → mejora). Así es como la salud digital pasa de pilotos a impacto a nivel poblacional. McKinsey & Company
La nueva investigación de McKinsey describe cómo las asociaciones público-privadas (APP) realmente escalon digitalmente la salud: comienza con una justificación clara (capacidad, escala o financiamiento), elige el actor privado adecuado, y diseña de antemano la propiedad, adquisición, privacidad de datos y sostenibilidad. Las lecciones de Canadá, Estonia, México, Tanzania y Togo muestran qué funciona—y por qué.
Puntos clave
Capacidad, escala, financiamiento: Los gobiernos suelen involucrar socios privados por sus capacidades técnicas únicas (100% de los casos), escala (83% en ecosistemas maduros) o financiamiento (48% en contextos limitados).
Upside económico comprobado: Las herramientas digitales pueden desbloquear hasta un 15% de eficiencia en los sistemas de salud de países de ingresos bajos y medios para 2030 al desplegarlas a gran escala.
Mecanismos reales, no eslóganes: La adquisición directa, centros de innovación, participaciones accionarias y la propiedad por fases ayudan a alinear incentivos y sostener soluciones.
Cinco lecciones que se repiten una y otra vez
Guía sobre dónde invertir. Usa un mapa de ruta nacional de salud digital y clarifica la propiedad para reducir la fragmentación (por ejemplo, Connect Care de Alberta con Epic).
Involucra al actor adecuado. Afya-tek de Tanzania mezcló herramientas para CHW y flujos de trabajo farmacéuticos al asociarse con D-tree/AHAI para obtener experiencia y financiamiento.
Crea incentivos. Reducciones fiscales, subvenciones y centros de innovación (por ejemplo, la comunidad HealthTech de Estonia; CAN Health en Canadá) aceleran la calidad y adquisición.
Construye confianza con salvaguardas. Aplica normas alineadas con el GDPR (Estonia PDPA) y requiere supervisión para acceder a conjuntos de datos sensibles (por ejemplo, biobanco FINBB).
Planea la sostenibilidad. Utiliza financiamiento no público donde sea necesario, participaciones accionarias para alinear incentivos (Unity Health Toronto × Signal 1), y transiciones de propiedad por fases (por ejemplo, m-mama, CHIS de Togo).
McKinsey también señala: el gasto del sector privado representa 40–60% del gasto en salud en muchos países de ingresos bajos y medianos, y la inversión privada en salud digital alcanzó los $25.1 mil millones en 2024—resaltando por qué las APP son importantes. McKinsey & Company
Pasos prácticos o ejemplos (un manual que puedes usar)
Comienza con el “por qué”. ¿Estás comprando capacidad (triaje de IA, implementación de EHR), escala (despliegue nacional) o financiamiento (capital combinado/donante)? Escribelo; esto guía la selección del modelo.
Elige el modelo.
Adquisición directa para sistemas críticos y estandarizados.
Centros de innovación y entornos de prueba para pruebas rápidas.
Modelos de acciones/cuotas para alinear incentivos para la IA co-desarrollada o análisis.
Decide propiedad y supervisión temprano. Separa la propiedad de la solución del IP, define la supervisión conjunta o única, y establece un camino de transición (privado→conjunto→público) para construir capacidad pública.
Desmitifica los datos desde el primer día. Codifica la privacidad, el acceso y la auditoría; enlaza la elegibilidad de adquisición con el cumplimiento de leyes/estándares nacionales.
Financiación para la durabilidad. Combina líneas presupuestarias con capital privado/donante; usa pagos diferidos o tarifas basadas en volumen para suavizar el flujo de efectivo.
Mide lo que importa. Rastrea la adopción (pacientes/profesionales de la salud), costos para servir, reducciones de tiempo de espera e impactos en la equidad; el manual de adopciones de McKinsey muestra las fases de configuración → escalamiento → mejora de beneficios que mejoran la adhesión.
Ejemplos vivos para hacerlo tangible
Receta electrónica de Estonia: nacional, integrada con EHR y sistemas nacionales—recetas digitales casi universales.
Unity Health Toronto × Signal 1 (Canadá): el hospital toma una participación minoritaria; actúa como un “laboratorio viviente” para monitoreo de IA (CHARTWatch).
COVID360 de Ciudad de México: asociación público-fundación para establecer rápidamente una plataforma de tratamiento durante COVID-19.
Tanzania Afya-tek: conecta a trabajadores de salud comunitarios, instalaciones y dispensarios—adquirido a través de un mapa de ruta; construido para interoperabilidad.
La última guía de McKinsey muestra que las asociaciones público-privadas escalan la salud digital cuando los gobiernos definen el “por qué”, eligen el actor privado adecuado, aseguran el financiamiento/propiedad, aplican salvaguardas de datos y planean para la sostenibilidad—utilizando mapas de ruta, incentivos y propiedad por fases para alcanzar la escala nacional. McKinsey & Company
Preguntas frecuentes
¿Qué son las asociaciones público-privadas en salud digital?
Colaboraciones estructuradas donde gobierno y actores privados (con y sin fines de lucro) co-diseñan, construyen u operan soluciones de salud digital—a menudo con financiamiento mixto y supervisión compartida. McKinsey & Company
¿Por qué estas asociaciones son importantes ahora?
Porque las brechas de capacidad, escala y financiamiento persisten—especialmente en países de ingresos bajos y medios donde el gasto privado es el 40–60% del gasto en salud y la inversión digital está en aumento. McKinsey & Company
¿Cómo funcionan las asociaciones en la práctica?
Los modelos comunes incluyen adquisición directa, centros de innovación, estructuras de acciones o tarifas y propiedad por fases; el éxito depende de la privacidad de datos, adquisición transparente y mapas de ruta claros. McKinsey & Company
¿Cuál es el valor potencial?
En países de ingresos bajos y medios, las herramientas digitales escaladas podrían desbloquear hasta 15% de ganancias de eficiencia del sistema; la OMS estima que incluso la inversión digital modesta por paciente puede salvar más de 2 millones de vidas por enfermedades no transmisibles con el tiempo. McKinsey & Company
Resumen
El mensaje de McKinsey es pragmático: trata las APP como problemas de diseño. Elige el modelo que coincida con tu “por qué”, incorpora gobernanza y privacidad, financia para el largo plazo y establece un mapa de ruta de adopción (configuración → escalamiento → mejora). Así es como la salud digital pasa de pilotos a impacto a nivel poblacional. McKinsey & Company
Recibe noticias y consejos sobre IA cada semana en tu bandeja de entrada
Al suscribirte, das tu consentimiento para que Generation Digital almacene y procese tus datos de acuerdo con nuestra política de privacidad. Puedes leer la política completa en gend.co/privacy.
Próximos talleres y seminarios web

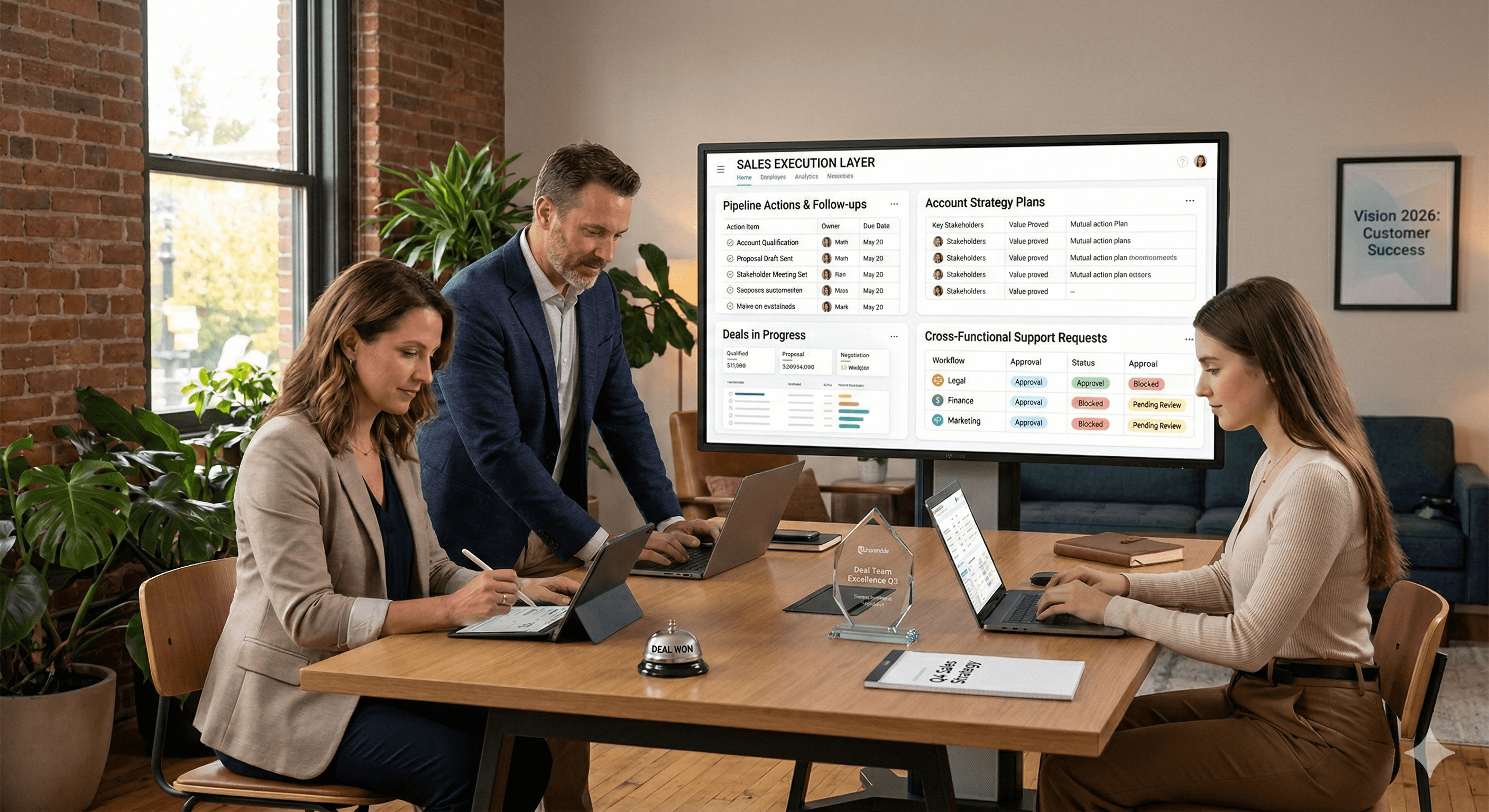
Claridad Operacional a Gran Escala - Asana
Webinar Virtual
Miércoles 25 de febrero de 2026
En línea

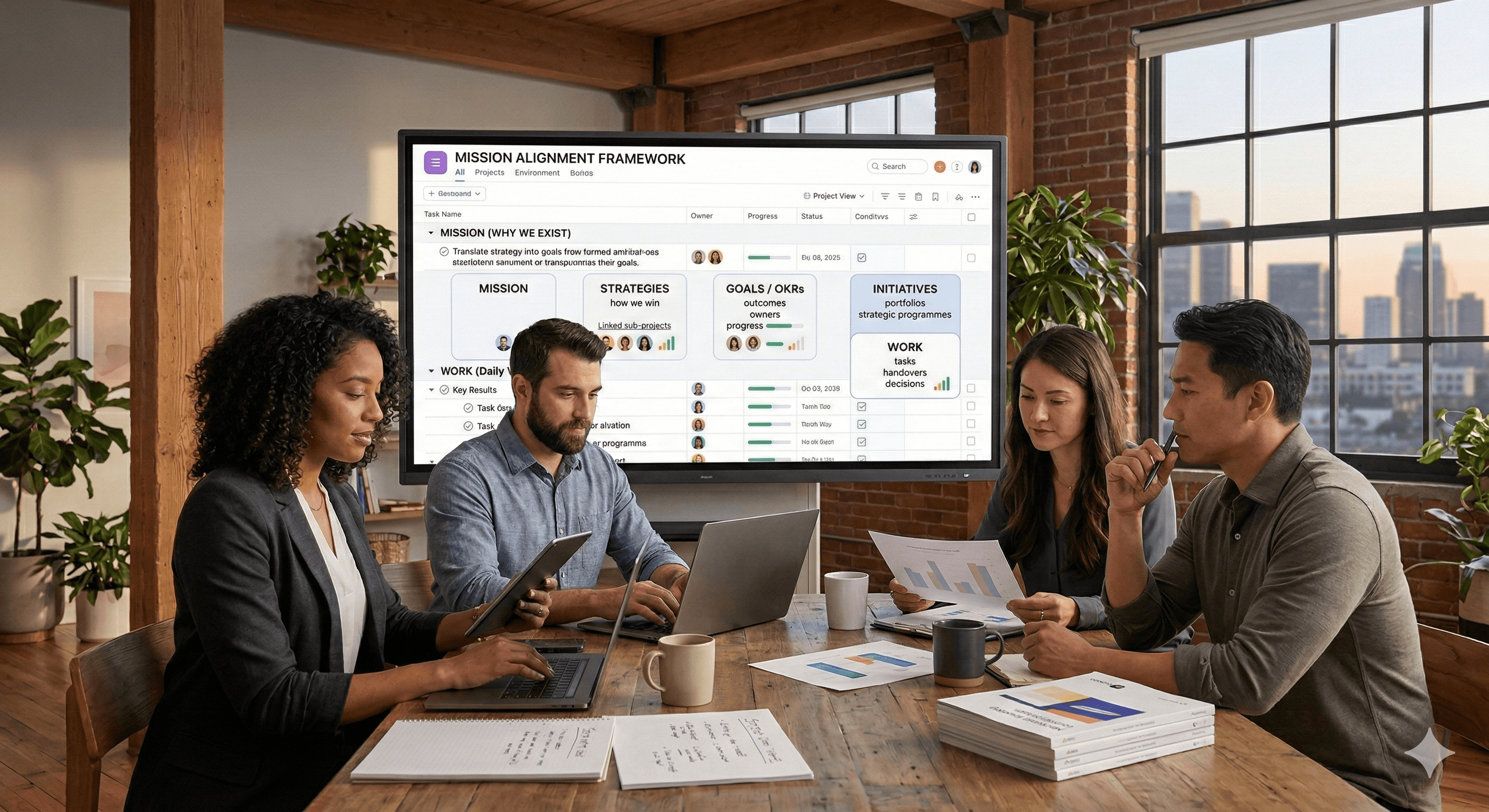
Trabaja con compañeros de equipo de IA - Asana
Taller Presencial
Jueves 26 de febrero de 2026
Londres, Reino Unido

De Idea a Prototipo: IA en Miro
Seminario Web Virtual
Miércoles 18 de febrero de 2026
En línea
Generación
Digital

Oficina en Reino Unido
Generation Digital Ltd
33 Queen St,
Londres
EC4R 1AP
Reino Unido
Oficina en Canadá
Generation Digital Americas Inc
181 Bay St., Suite 1800
Toronto, ON, M5J 2T9
Canadá
Oficina en EE. UU.
Generation Digital Américas Inc
77 Sands St,
Brooklyn, NY 11201,
Estados Unidos
Oficina de la UE
Software Generación Digital
Edificio Elgee
Dundalk
A91 X2R3
Irlanda
Oficina en Medio Oriente
6994 Alsharq 3890,
An Narjis,
Riad 13343,
Arabia Saudita
Número de la empresa: 256 9431 77 | Derechos de autor 2026 | Términos y Condiciones | Política de Privacidad
Generación
Digital

Oficina en Reino Unido
Generation Digital Ltd
33 Queen St,
Londres
EC4R 1AP
Reino Unido
Oficina en Canadá
Generation Digital Americas Inc
181 Bay St., Suite 1800
Toronto, ON, M5J 2T9
Canadá
Oficina en EE. UU.
Generation Digital Américas Inc
77 Sands St,
Brooklyn, NY 11201,
Estados Unidos
Oficina de la UE
Software Generación Digital
Edificio Elgee
Dundalk
A91 X2R3
Irlanda
Oficina en Medio Oriente
6994 Alsharq 3890,
An Narjis,
Riad 13343,
Arabia Saudita