AI for Healthcare Efficiency with Glean
AI for Healthcare Efficiency with Glean
AI
Glean
Dec 19, 2025


Not sure where to start with AI?
Assess readiness, risk, and priorities in under an hour.
Not sure where to start with AI?
Assess readiness, risk, and priorities in under an hour.
➔ Download Our Free AI Readiness Pack
Why efficiency is a global clinical safety issue
Administrative burden is universal; automation delivers measurable savings. The CAQH Index estimates that digitising and automating high-friction US transactions could save $15B+ annually, largely by removing manual eligibility, status, and authorization steps.
At the same time, policy moves are accelerating: the CMS Interoperability & Prior Authorization Final Rule sets API and turnaround obligations (standard prior auth in 7 days; 72 hours expedited) with major deadlines in 2026–2027 for impacted payers—driving process redesign now.
Globally, digital health adoption remains a priority across regions (EU/WHO), but capacity constraints mean tools that remove admin friction create outsized impact.
Where AI helps most (and how Glean fits)
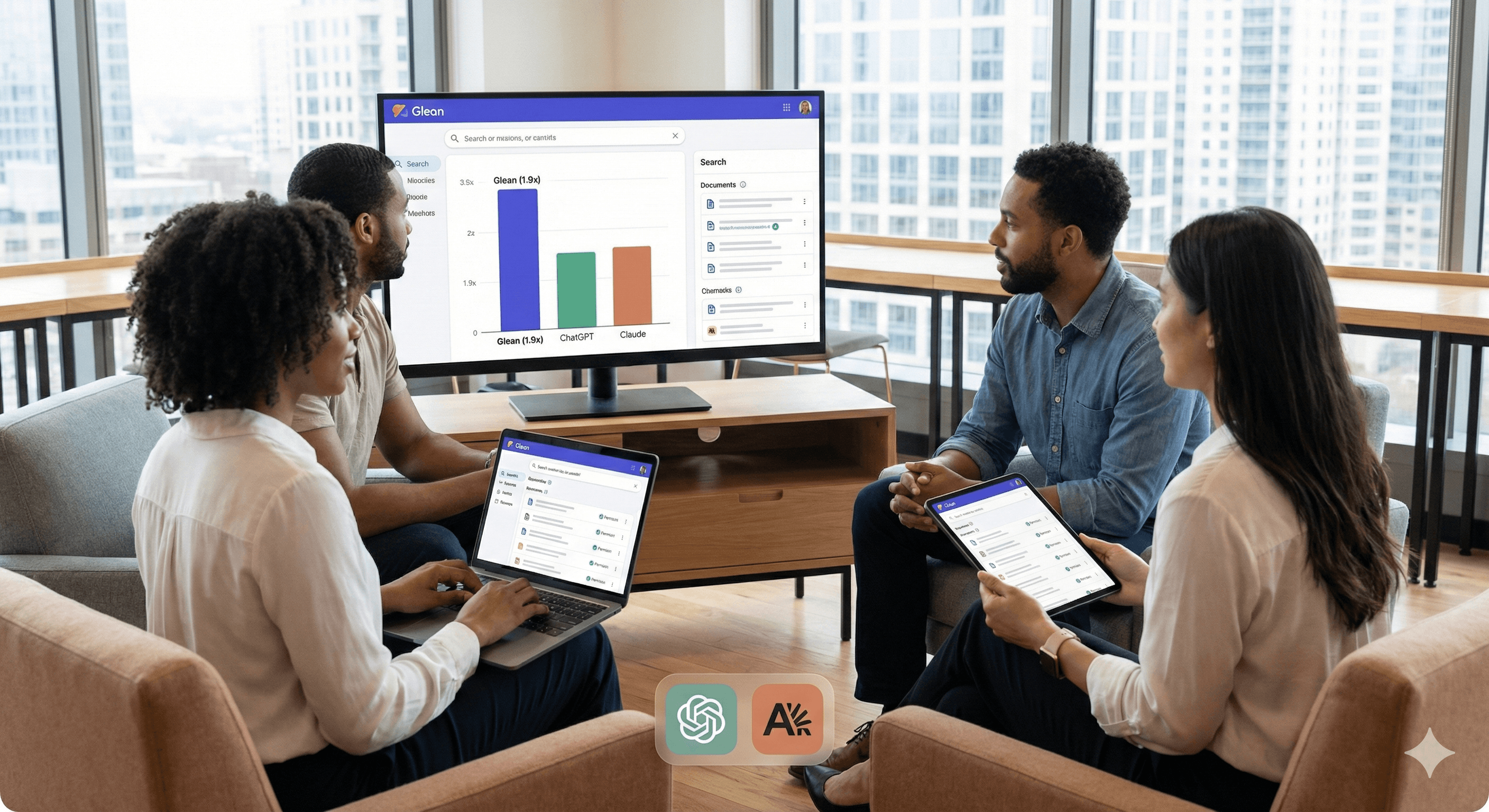
1) Knowledge in flow of work (search + assistant)
Clinicians and non-clinical teams lose time hunting for policies, payer bulletins, referral and prior-auth steps, and runbooks. Glean indexes approved sources (SharePoint/Google Drive/Confluence; ServiceNow/Salesforce/Zendesk) and returns permission-aware answers with citations in Teams/Slack and ticket sidebars—reducing escalations and handle time.
2) Fewer avoidable denials (agents + revenue cycle checks)
Many denials trace to documentation gaps and policy mismatches. AI agents can pre-check draft claims against payer rules, flag missing elements, and route edge cases for human review—improving clean-claim rates and cash flow. CAQH’s data underscores the financial upside of automating these transactions.
US context: Align pre-submission checks to CMS prior-auth and attachment workflows so providers aren’t caught by the 7-day/72-hour clocks as APIs roll out.
3) Staff self-service and service operations
From IT/HR to estates and rota queries, AI deflects repetitive questions and accelerates triage so clinicians spend less time on administration and more on care.
Security, privacy, and regional compliance (board-ready)
Foundational controls: Glean publishes security practices and certifications (SOC 2 Type II, ISO 27001) and states alignment to HIPAA and GDPR, with permission-mirroring so results respect source access.
United States (HIPAA): Ensure Business Associate considerations, map safeguards to the Privacy/Security Rules, and track the 2025 NPRM proposing stronger controls (e.g., MFA, encryption, incident response).
Canada (PHIPA/PIPEDA): For Ontario providers/insurers, PHIPA AMPs are now in force; PIPEDA applies to private-sector personal information processing nationally—align audit trails and consents.
90-Day rollout (global pattern you can localise)
Phase 1 — Foundation (Weeks 1–3)
Prioritise journeys: top denial reasons, top prior-auth procedures, top 50 staff queries.
Connect core sources (M365/SharePoint, Confluence, ServiceNow, Salesforce, Zendesk).
Enable citations and permission sync; define retention/telemetry behaviours per region.
Phase 2 — Assist in-flow (Weeks 4–8)
Roll out the assistant in Teams/Slack and ticket sidebars.
Stand up two agents: (1) prior-auth checklist builder; (2) claim/charge pre-submission audit. Track clean-claim %, touches per claim, and turnaround.
Phase 3 — Govern & scale (Weeks 9–12)
Adopt an “AI formulary”: approved prompts, data sources, exception paths.
Map evidence to HIPAA/PHIPA/PDPL artefacts and—where relevant—CMS prior-auth reporting.
Example impact by workflow
Area | Common friction | AI approach | Expected impact |
|---|---|---|---|
Prior authorisation (US) | Fragmented payer rules, missing docs | Agent assembles payer-specific checklists; validates packages before submission | Faster scheduling, fewer returns. cms.gov+1 |
Coding & claims | Late discovery of errors | Pre-submission scan vs. rules; route edge cases | Higher clean-claim rate, lower rework. caqh.org |
Staff self-service | Policy hunting, rota/IT queries | Permission-aware answers in Teams/Slack/portal with sources | Time back to care; fewer tickets. docs.glean.com |
FAQs
How does AI streamline healthcare operations?
By removing search time and automating routine checks. Staff get trusted answers in-flow, while agents validate authorisations and claims up front—freeing capacity for patient care. docs.glean.com+1
What role does AI play in reducing denials?
Most denials stem from documentation and policy mismatches. AI agents flag gaps before submission and align to payer rules, improving clean-claim rates and reimbursement speed. caqh.org
Is AI adoption secure in healthcare settings?
Yes—when paired with strong controls. Glean documents SOC 2/ISO practices and alignment to HIPAA/GDPR, while regional laws (PHIPA, PDPL) require auditable access and governance you can evidence. LawNow+3Glean+3Glean+3
Summary
Across regions, the fastest wins are administrative: find the right guidance in-flow, prevent avoidable denials, and deflect repetitive requests. Glean’s Work AI platform delivers those wins with permission-aware search, assistants, and targeted agents—wrapped in controls your compliance teams can evidence under HIPAA/PHIPA/PDPL. Ready to tailor a rollout? Let’s talk.
Why efficiency is a global clinical safety issue
Administrative burden is universal; automation delivers measurable savings. The CAQH Index estimates that digitising and automating high-friction US transactions could save $15B+ annually, largely by removing manual eligibility, status, and authorization steps.
At the same time, policy moves are accelerating: the CMS Interoperability & Prior Authorization Final Rule sets API and turnaround obligations (standard prior auth in 7 days; 72 hours expedited) with major deadlines in 2026–2027 for impacted payers—driving process redesign now.
Globally, digital health adoption remains a priority across regions (EU/WHO), but capacity constraints mean tools that remove admin friction create outsized impact.
Where AI helps most (and how Glean fits)
1) Knowledge in flow of work (search + assistant)
Clinicians and non-clinical teams lose time hunting for policies, payer bulletins, referral and prior-auth steps, and runbooks. Glean indexes approved sources (SharePoint/Google Drive/Confluence; ServiceNow/Salesforce/Zendesk) and returns permission-aware answers with citations in Teams/Slack and ticket sidebars—reducing escalations and handle time.
2) Fewer avoidable denials (agents + revenue cycle checks)
Many denials trace to documentation gaps and policy mismatches. AI agents can pre-check draft claims against payer rules, flag missing elements, and route edge cases for human review—improving clean-claim rates and cash flow. CAQH’s data underscores the financial upside of automating these transactions.
US context: Align pre-submission checks to CMS prior-auth and attachment workflows so providers aren’t caught by the 7-day/72-hour clocks as APIs roll out.
3) Staff self-service and service operations
From IT/HR to estates and rota queries, AI deflects repetitive questions and accelerates triage so clinicians spend less time on administration and more on care.
Security, privacy, and regional compliance (board-ready)
Foundational controls: Glean publishes security practices and certifications (SOC 2 Type II, ISO 27001) and states alignment to HIPAA and GDPR, with permission-mirroring so results respect source access.
United States (HIPAA): Ensure Business Associate considerations, map safeguards to the Privacy/Security Rules, and track the 2025 NPRM proposing stronger controls (e.g., MFA, encryption, incident response).
Canada (PHIPA/PIPEDA): For Ontario providers/insurers, PHIPA AMPs are now in force; PIPEDA applies to private-sector personal information processing nationally—align audit trails and consents.
90-Day rollout (global pattern you can localise)
Phase 1 — Foundation (Weeks 1–3)
Prioritise journeys: top denial reasons, top prior-auth procedures, top 50 staff queries.
Connect core sources (M365/SharePoint, Confluence, ServiceNow, Salesforce, Zendesk).
Enable citations and permission sync; define retention/telemetry behaviours per region.
Phase 2 — Assist in-flow (Weeks 4–8)
Roll out the assistant in Teams/Slack and ticket sidebars.
Stand up two agents: (1) prior-auth checklist builder; (2) claim/charge pre-submission audit. Track clean-claim %, touches per claim, and turnaround.
Phase 3 — Govern & scale (Weeks 9–12)
Adopt an “AI formulary”: approved prompts, data sources, exception paths.
Map evidence to HIPAA/PHIPA/PDPL artefacts and—where relevant—CMS prior-auth reporting.
Example impact by workflow
Area | Common friction | AI approach | Expected impact |
|---|---|---|---|
Prior authorisation (US) | Fragmented payer rules, missing docs | Agent assembles payer-specific checklists; validates packages before submission | Faster scheduling, fewer returns. cms.gov+1 |
Coding & claims | Late discovery of errors | Pre-submission scan vs. rules; route edge cases | Higher clean-claim rate, lower rework. caqh.org |
Staff self-service | Policy hunting, rota/IT queries | Permission-aware answers in Teams/Slack/portal with sources | Time back to care; fewer tickets. docs.glean.com |
FAQs
How does AI streamline healthcare operations?
By removing search time and automating routine checks. Staff get trusted answers in-flow, while agents validate authorisations and claims up front—freeing capacity for patient care. docs.glean.com+1
What role does AI play in reducing denials?
Most denials stem from documentation and policy mismatches. AI agents flag gaps before submission and align to payer rules, improving clean-claim rates and reimbursement speed. caqh.org
Is AI adoption secure in healthcare settings?
Yes—when paired with strong controls. Glean documents SOC 2/ISO practices and alignment to HIPAA/GDPR, while regional laws (PHIPA, PDPL) require auditable access and governance you can evidence. LawNow+3Glean+3Glean+3
Summary
Across regions, the fastest wins are administrative: find the right guidance in-flow, prevent avoidable denials, and deflect repetitive requests. Glean’s Work AI platform delivers those wins with permission-aware search, assistants, and targeted agents—wrapped in controls your compliance teams can evidence under HIPAA/PHIPA/PDPL. Ready to tailor a rollout? Let’s talk.
Get weekly AI news and advice delivered to your inbox
By subscribing you consent to Generation Digital storing and processing your details in line with our privacy policy. You can read the full policy at gend.co/privacy.
Upcoming Workshops and Webinars


Operational Clarity at Scale - Asana
Virtual Webinar
Weds 25th February 2026
Online


Work With AI Teammates - Asana
In-Person Workshop
Thurs 26th February 2026
London, UK


From Idea to Prototype - AI in Miro
Virtual Webinar
Weds 18th February 2026
Online
Generation
Digital

UK Office
Generation Digital Ltd
33 Queen St,
London
EC4R 1AP
United Kingdom
Canada Office
Generation Digital Americas Inc
181 Bay St., Suite 1800
Toronto, ON, M5J 2T9
Canada
USA Office
Generation Digital Americas Inc
77 Sands St,
Brooklyn, NY 11201,
United States
EU Office
Generation Digital Software
Elgee Building
Dundalk
A91 X2R3
Ireland
Middle East Office
6994 Alsharq 3890,
An Narjis,
Riyadh 13343,
Saudi Arabia
Company No: 256 9431 77 | Copyright 2026 | Terms and Conditions | Privacy Policy
Generation
Digital

UK Office
Generation Digital Ltd
33 Queen St,
London
EC4R 1AP
United Kingdom
Canada Office
Generation Digital Americas Inc
181 Bay St., Suite 1800
Toronto, ON, M5J 2T9
Canada
USA Office
Generation Digital Americas Inc
77 Sands St,
Brooklyn, NY 11201,
United States
EU Office
Generation Digital Software
Elgee Building
Dundalk
A91 X2R3
Ireland
Middle East Office
6994 Alsharq 3890,
An Narjis,
Riyadh 13343,
Saudi Arabia